Presented by Bongiovi Medical & Health Technologies and AudioLab360. Learn more about our approach to audio in medicine and beyond.

Authors
- Thomas Haffey DO FACC
- Daniel Weiss MD FACC BSEE
- Jim Hughes MD FACS
- Joseph Butera III
- David Lopez Jr
- Aashka Shah
- Keren Fishman
- Rajat Mohanka
Presenting a cost-effective screening tool for significant carotid artery disease at the patient’s bedside.
Background
Carotid atherosclerosis is ubiquitous and carries numerous serious sequelae, including embolic cerebrovascular phenomena (TIA, stroke). Early detection and intervention are essential components of managing the disease. The current screening routine includes stethoscopic auscultation to listen for carotid bruits. Detecting the presence of carotid bruits using a conventional stethoscope carries a sensitivity of only 53% and a specificity of 85%. We assessed a novel digital stethoscope’s ability to detect significant carotid stenosis >50% (SCS).
Scope of the Problem
- Carotid atherosclerosis is ubiquitous and carries with it numerous serious sequelae, including embolic cerebrovascular phenomena (TIA, stroke)
- Early detection and intervention are essential components of managing the disease.
- The current screening routine includes stethoscope auscultation to listen for carotid bruits.
- Detecting the presence of carotid disease using a standard stethoscope:
- Sensitivity: 53%
- Specificity: 85%
- Can improvements be made in stethoscope hardware to better detect bruits?
- Can the acoustic signature be analyzed to provide quantitative metrics similar to costly ultrasound procedures?
Methods
Using the Aria carotid stethoscope (Bongiovi Acoustic Labs, Port St Lucie, FL) all patients had carotid recordings made right and left sides, then underwent carotid ultrasound imaging.
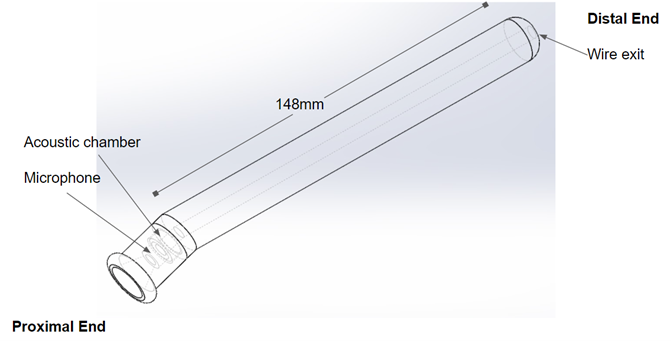
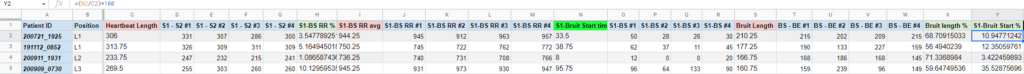
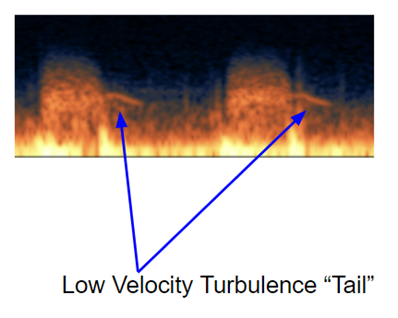
The recordings were processed digitally using Bongiovi MDPS software (Bongiovi) and then spectrographically analyzed to derive the percent bruit onset time (PBOT) fig.1 and bruit “shape” fig.2. MDPS audio processing was used primarily to improve the audibility of carotid acoustic features and improve spectrographic visualization.
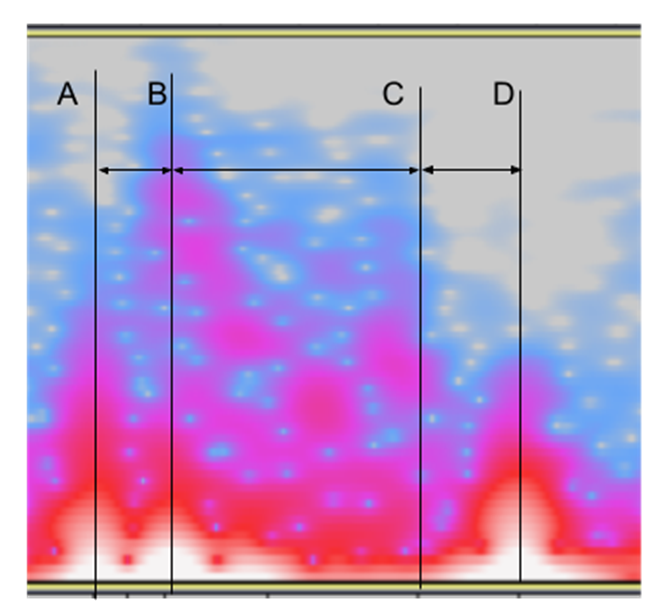
Figure 1 represents the method used to analyze a bruit’s timing characteristics. The vertical lines labeled A, B ,C, D indicate specific time stamps within the audio file:
- A = S1 start of systole
- B = Onset of bruit
- C = End of bruit
- D = S2 end of systole / start of diastole
The intervals between these points in the audio file are derived by subtracting an earlier time stamp from a later one. Intervals were measured for four consecutive heartbeats and averaged.
Useful algorithms were derived by searching for patterns in the timing that correlated with percent stenosis.
By normalizing the bruit onset time (B minus A) as a percentage of systole (D minus A), we arrive at PBOT:
- Systole Time(ms) S = D – A
- Bruit Onset Time(ms) R = B – A
- PBOT(%) = (R / S) * 100
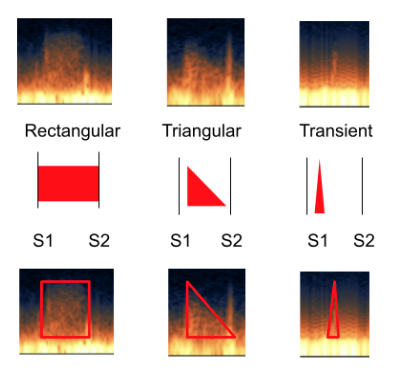
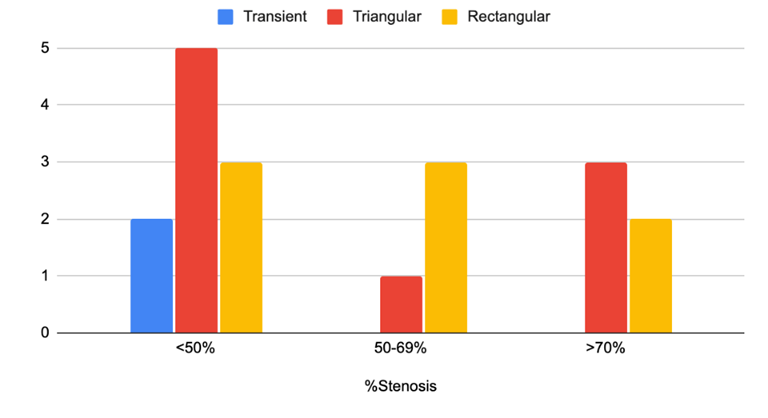
Many correlations between acoustic properties and the percentage of stenosis were evaluated. One method that yielded improved accuracy was the classification of bruit “shape” as it appears in the spectrogramfig.2.
Results
There were 124 patients, with 248 carotid recordings made. 19 bruits were detected in 15 patients (4 had bilateral bruits). Ultrasound results were compared with auscultation results to create performance metrics. Only 2 carotids with >50% stenosis had no bruit (predictive negative value 99%). In those carotids with bruits, if PBOTfig.4 was <9.5%, the sensitivity for SCS was 100%, with a specificity of 80%. When bruit “shape”fig.2 was included as a differentiating metricfig.3, specificity was 90%.
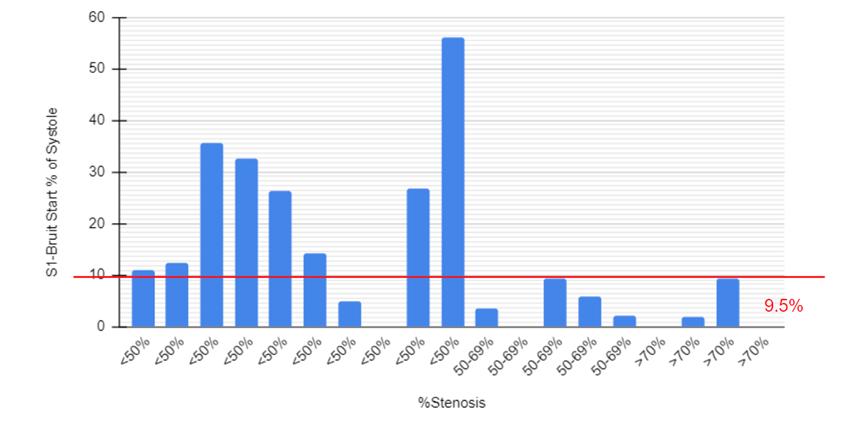
- PBOT Only
- True Positive = >50% and PBOT <9.5%
- True Negative = <50% stenosis and PBOT >=9.5%
- Sensitivity: 100%
- Specificity: 80%
- PBOT and Bruit Shape
- True Positive = >50% and PBOT <9.5% and NOT transient shape
- True Negative = <50% stenosis and PBOT >=9.5%
- Sensitivity: 100%
- Specificity: 90%
Conclusion
The absence of a carotid bruit heard using the novel sound acquisition device (NSAD) confers a <2% chance of the presence of Significant Carotid Stenosis (SCS). For those carotids with bruits, PBOT can differentiate among those with SCS vs those without SCS with 100% sensitivity and high specificity. Thus, using NSAD with PBOT analysis may be a useful SCS screening tool.
Discussion
Understanding further inquiry is required to fine-tune and validate the methods; this study provides a strong signal of efficacy. Ongoing study of this method would include increasing the number of bruits for analysis for three cohorts; less than 50% stenosis, greater than 50%, and greater than 70%. We expect the PBOT threshold to shift from 9.5% as we analyze ROC curves with larger data sets. We expect the sensitivity and specificity to regress to an appropriate mean as the data size increases.
This bedside screening tool is essential to a comprehensive stroke risk management system. As an electronic stethoscope, this technology is well suited for telemedicine applications with obvious automation using current machine learning methods.
Presented by Bongiovi Medical & Health Technologies and AudioLab360. Learn more about our approach to audio in medicine and beyond.